By Countercurrents Collective
The U.S. state and local public health offices are scrambling to respond to the coronavirus outbreak. They are doing so against a backdrop of years-long budget cuts, leaving them without the trained employees or updated equipment to adequately address the virus’ growing threat, former public health officials say.
A USA Today report said:
“In the last 15 years, public health, the country’s frontline defense in epidemics, lost 45% of its inflation-adjusted funding for staff, training, equipment and supplies. The Public Health Emergency Fund, created for such disease or disaster relief is long depleted. And much of the money the federal government is racing to come up with now to combat the COVID-19 outbreak will be pulled from other often-dire health needs and likely will arrive too late to hire the needed personnel.
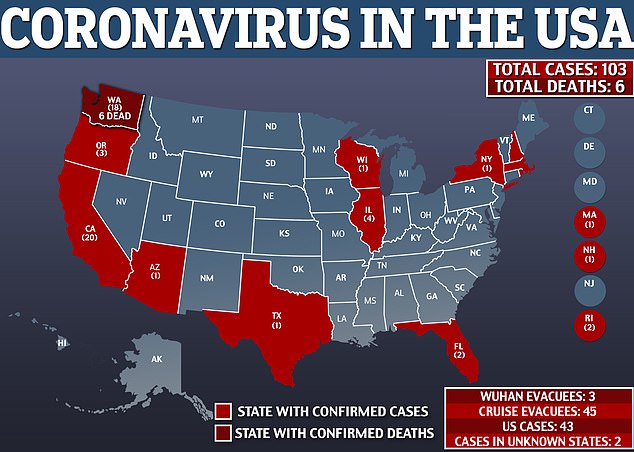
“Florida, with two cases so far, and Washington, where six deaths have been reported, have declared states of emergency, and state and local officials there and elsewhere assure they have staff, equipment and procedures ready. But early testing glitches in California, the failure to protect federal health officials from the virus in cruise ship patients, and a climbing number of U.S. cases raise questions about that confidence.
“Health and Human Services Secretary Alex Azar told a Senate panel last week there are only about 30 million of the 300 million face masks needed for health care workers.
“‘Once again, we’re not that prepared,’ said Dr. Boris Lushniak, a former deputy and acting U.S. Surgeon General who spent 13 years at the Centers for Disease Control and Prevention and is now dean of University of Maryland’s School of Public Health. ‘When those (basic public health efforts) aren’t supported well, in the time of emergency you don’t have the infrastructure to shift gears and go into emergency mode.’”
According to the report, the prospect of contending with an epidemic hits often-ignored public health departments already taxed by at least 70 homegrown threats, including a host of sexualy transmitted diseases and tuberculosis.
The report said:
“It’s been 16 months since President Donald Trump declared opioid abuse a ‘public health emergency,’ and less than a year since Kentucky warned it might have to close 42 of its county health departments amid the country’s worst outbreak of Hepatitis A. In New York City, an explosion of measles among unvaccinated children that ended just six months ago cost the city more than $2 million to fight and involved 400 public health employees, according to the Big Cities Health Coalition.
“Such health crises come on the heels of massive cuts to state and local public health budgets that started during the recession, and saw funding steadily decrease. Public health funding fell from more than $900 million in fiscal year 2005 to $675 million in fiscal year 2020, a drop of 25% or 45% when adjusted for inflation.
“Public health represented 2.5% – or just $274 per person – of all U.S. health spending in the country in 2017, according to the nonprofit Trust for America’s Health.”
It said:
“‘The nation’s ability to be prepared has been eroded in an enormous way,’ said Dr. Rahul Gupta, West Virginia’s former health secretary and now chief medical officer at the March of Dimes. ‘It’s really unbelievable that it’s happening when we have a higher frequency of these risks’ of global novel virus transmission.’”
The report added:
“The U.S. President Trump last week asked Congress to approve $2.5 billion for coronavirus response efforts that includes $1 billion for vaccine research. Democratic Senate Minority Leader Charles Schumer proposed $8.5 billion, including $2 billion that would repay state and local governments. No matter what amount is ultimately approved by Congress, the money will come from other health areas and much of it likely will take months wend its way through the federal Department of Health and Human Services to states and then local health departments.
“Another $136 million in funding cuts from other HHS agencies, including $37 million from heating assistance for low income families and $4.9 million from the Substance Abuse and Mental Health Administration, is now being transferred to states, HHS spokeswoman Caitlin Oakley said Friday.”
The report cited Brian Castrucci, an epidemiologist who spent a decade in the health departments for Texas, Georgia and Philadelphia: As a pandemic looms “is not the time to have the conversation” about funding health departments.
According to the report, Brian Castrucci has little faith Congress and White House officials will learn from their funding mistakes and make changes after the coronavirus outbreak ends. “While we are waiting, people are getting sick and the response doesn’t wait,” said Castrucci, now CEO of the deBeaumont Foundation. “We don’t have the luxury, working in public health, to wait for money to come.”
The report said:
“Trust for America’s Health, an illness and injury-focused nonprofit with funders including the Robert Wood Johnson Foundation and W.K. Kellogg Foundation, found it took six weeks for funding to get approved by Congress for the Ebola outbreak, seven weeks for H1N1 in 2009-2010 and seven months for Zika, which struck the U.S. in early 2016.
“Counties wracked by opioids in states including West Virginia, Indiana and Ohio – all ranked by Trust for America’s Health among the 13 least prepared states for a public health emergency – now have to prepare for the possibility of airline passengers needing immediate isolation in hotels and relying on state and federal money redirected from other pressing needs.
“Still, in Indiana, which also ranks 49th on one list of public health funding, Health Secretary Kristina Box said the state is ‘very supported in this and not feeling that we are lacking any funds to address this issue.’
“In the state’s Marion County, however, health department director Dr. Virginia Caine warned ‘a major crisis or a major number of cases’ could be a different story.
“‘I might be concerned that we may not have enough protective equipment, surgical masks, things of that nature, where our stockpile we might want to have be a little bit larger,’ said Caine.
“In Ohio, Columbus’ Public Health Commissioner Dr. Mysheika Roberts said if anyone is to blame for a lack of preparedness, it’s the federal government as it determines most of the funding for local health departments. She called Washington’s decisions ‘unfortunate’ but said the state’s larger cities were well positioned for a possible outbreak.
“A day before Washington announced its first coronavirus death Saturday, Seattle and King County health department policy director Ingrid Ulrey said the cost of responding to the outbreak already was daunting. Diverting staff to coronavirus and overtime already had cost about $200,000 more a week – about 5% of the department’s budget.
“Ulrey said the office plans to hire a temporary team of workers for about eight months at an estimated cost of least $1.25 million. The additional cost could be two or three times that if there are ‘many many cases.’
“‘This is not sustainable,’ she said.
“Time is also a problem, said Oscar Alleyne, program director at the National Council of County and Local Health Officials. State and local health departments have lost about 30,000 people over the last seven years, he said, and now have to find or wait for money to hire recent public health graduates and train them for these new, often short-term jobs.
“It takes six to nine months to find and hire the people capable of doing the testing and other surveillance work needed, said Dr. Lamar Hasbrouck, a former CDC medical epidemiologist, who was Illinois’ health secretary from 2012 to 2015.”
The report added:
“Dr. Nirav Shah, who served as New York’s state health commissioner from 2011 to 2014, said in addition to supplies and other department resources funding will be needed for staff to perform tracing of the contacts of infected people. He worries most about cuts to Epidemiological Intelligence Service, which can go straight to the source of the virus.
‘The issue is we are becoming more reactive and less proactive,’ said Shah, now a senior scholar at Stanford University’s Clinical Excellence Research Center. ‘We are waiting for people to cross the border, rather than going to the source.”
The report said:
“When it comes to public health, those with intravenous drug addictions are most visibly impacted due to the need for needle exchanges or other measures to stop the spread of Hepatitis A or HIV.
“Gupta called it ‘morally unjustifiable,’ to move funding, as the administration is, from programs such as addiction prevention at the Substance Abuse and Mental Health Administration.
“‘What we shouldn’t do is take from one set of a vulnerable population to address another,’ he said.
“Hasbrouck, who was involved in responses to H1N1, the Middle East respiratory syndrome (MERS) and Ebola, also worried about patients dealing with other diseases, including those with HIV on Medicaid and other government-supported health insurance coverage.
“‘You’re robbing Peter to pay Paul and never made whole,’ said Hasbrouck, who now works as a public health consultant. ‘And you’ve lost time and can’t get that time back.’
“The health care system relies on public health agencies.
“In a full-blown outbreak, coronavirus patients will be spread across many hospitals that are normally competitors, so public health agencies have to be the connective tissue that binds and coordinates the response, said Dr. Tom Talbot, the chief hospital epidemiologist at Vanderbilt University Medical Center.
“‘They are my heroes,” said Talbott, “because they are drastically underfunded and still on the front lines helping to fight this thing.’”
Vice President Mike Pence has reassured that Americans despite the rise in the number of cases and deaths over the last few days, the risk to Americans remains low.
There are currently no plans to restrict travel within the United States, but Pence said there will be 100% screening for people who travel to the U.S. from Italy and South Korea.
NY governor pushes insurers to waive coronavirus related fees
Other media reports said:
New York Governor Andrew Cuomo announced a new directive Monday night that requires New York state health insurers to waive the cost to their clients for any procedure related to testing for coronavirus, including emergency room, urgent care and office visits.
The state’s Medicaid recipients will not be expected to pay or co-pay for any COVID-19 related testing, under the directive.
Passengers’ travel history
Airlines are being instructed by the U.S. federal government to ask if their U.S.-bound passengers have visited China or Iran in the last two weeks, according to the Transportation Security Administration. Carriers are encouraged to look through reservations and passport stamps if necessary, agency officials said.
If a passenger traveled to one of those countries in the last 14 days, they will have to enter through one of the 11 airports designated by the Department of Homeland Security where they will be screened for the virus.
Trump touts additional travel restrictions
President Trump told reporters there would be additional travel restrictions to countries with ongoing outbreaks, but he did not provide specifics.
“We’re doing that, we’ve already done it with three countries in addition to China,” he said.
Over the weekend, Trump said a vaccine is being developed “very quickly” and “very rapidly.” However, Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, cautioned last week that the process is likely to take “about a year to a year and a half.”
Panic buying
Numerous grocery and supply stores in the U.S. recorded panic buying on February 29.
Shoppers in a Costco in Seattle, Washington, stood in long lines on February 29 to buy essential items like water and toilet paper in preparation for potential coronavirus quarantines.
Shoppers filled bulk goods stores like Costco over the weekend to stock up on water and food amid concerns that Americans will soon be under a coronavirus quarantine.
Reports of long lines and empty shelves came on social media and in local news, though experts say that there is no need to panic, and that stocking up is not necessary.
At the Brooklyn Costco, shoppers lined up outside the store before it opened on Sunday to pick up water and food, the New York Post reported.
“The coronavirus has them panicked … they think the world is coming to an end,” the store’s manager told the outlet. “This is great for business, though!”
Out on the west coast, the scene was similar. At a Los Angeles Costco, general manager Thad Kleszcz said the number of shoppers shot up on Friday and Saturday, after the first death in the U.S. was reported in Washington state.
“Antiseptic wipes and Clorox disinfecting wipes are flying out of here,” he told the Los Angeles Times. “We can’t keep those in stock.”
Dr. Robert Redfield, the director of the Centers for Disease Control, told Congress on Thursday that healthy Americans do not need to stock up on supplies at this time.
And there are no concerns right now that the U.S. will run out of water or food as the disease spreads worldwide.
The one item that is selling out, though, is face masks. Online and brick-and-mortar retailers like Amazon and Home Depot are out of masks, and health care professionals who need the masks are having trouble purchasing them.
The shortage led U.S. Surgeon General Jerome M. Adams to urge Americans to “STOP BUYING MASKS.”
“Seriously people- STOP BUYING MASKS! They are NOT effective in preventing general public from catching #Coronavirus, but if healthcare providers can’t get them to care for sick patients, it puts them and our communities at risk!” he posted on Twitter Saturday.
“The best way to protect yourself and your community is with everyday preventive actions, like staying home when you are sick and washing hands with soap and water, to help slow the spread of respiratory illness,” he added. “Get your #FluShot– fewer flu patients = more resources for #COVID19.”
Amazon said they have since removed tens of thousands of deals from sellers who had raised prices on the masks they still had in stock, and were not adhering to the site’s “fair pricing” guidelines.
“We have absolutely enforced the policy,” an Amazon spokesperson told CBS. “We identify them and quickly take action.”
Trump’s false assurances on coronavirus
Associated Press made a fact check on March 3, 2020, which is the following:
President Donald Trump persisted Monday in making false assurances about U.S. preparedness for the coronavirus outbreak and the prospects for a quick vaccine, or even cure.
In remarks at the White House and an evening rally in North Carolina, Trump reached for silver linings as the number of cases and deaths in the U.S. grew.
TRUMP: “We’re talking about a vaccine. Maybe a cure is possible. But we’re talking about a vaccine and they’re moving along very quickly, all of the pharmaceutical companies, are moving along very quickly.” — remarks before a meeting with Colombian President Iván Duque.
TRUMP: The U.S. may have a vaccine “relatively soon” and “something that makes you feel better … sooner.” — rally.
THE FACTS: That is misleading, given the far more cautious pronouncements of federal public-health officials and scientists. They say a vaccine is probably more than a year away at best and there are no special treatments for COVID-19. The notion of a quick “cure” is not in their vocabulary as they focus on trying to help people avoid getting the disease in the first place.
What’s actually happening: Studies have begun in COVID-19 patients in parts of the world to see if certain antiviral medications could help treat the infection.
Today, there are no proven treatments. In China, scientists have been testing a combination of HIV drugs against the new coronavirus, as well as an experimental drug named remdesivir that was in development to fight Ebola. In the U.S., the University of Nebraska Medical Center also began testing remdesivir, in some Americans who were found to have COVID-19 after being evacuated from a cruise ship in Japan.
It is not known how soon such studies will answer whether any of the drugs help. And many patients recover without needing any treatment. The biggest concern is how to help the fraction who become severely ill.
TRUMP: The U.S. is “ranked by far No. 1 in the world for preparedness” — rally.
THE FACTS: Not “by far.”
He is referring, as he did explicitly last week, to a report coauthored by Johns Hopkins Centers for Health Security. Hopkins experts on Monday said the U.S. got a “grade” that overall was highest by a few points among other high-income countries – Britain, Canada, Australia, countries in northern Europe – that are all at about the same level of preparedness.
But the report’s overall finding: “No country is fully prepared for an epidemic or pandemic,” cautioned Hopkins’ Jennifer Nuzzo, who coauthored the report.
It is difficult to say from the report that a country that scores 2 points higher than another is going to fare much better, she added.
Now that the new coronavirus is spreading around the world, Nuzzo’s biggest concern is the readiness of health care systems around the globe. There has been a lot of work in recent years to shore up public health capacity and strengthen laboratories and surveillance for dangerous new outbreaks.
But she said her report uncovered that few have paid attention to whether they have enough doctors and nurses, if those workers are seeing patients in a way that’s safe and if they have enough of the masks and other gear to safely do their jobs.
“We have seen time and time again in outbreaks that systems, that health systems that are unprepared often serve as points that amplify transmission to the community,” she said.
In the U.S., the biggest worry is access to that health care. “If fear of the cost of health care is a deterrent that could create a bad situation where people stay at home, potentially infecting others.”