February 6 marks the International Day of Zero Tolerance for Female Genital Mutilation (FGM), a practice affecting over 230 million girls and women worldwide and considered by the UN a grave violation of human rights.
FGM includes all procedures involving partial or total removal of the external female genitalia or any other injury to female genital organs for non-medical reasons. The WHO distinguishes four main types, from clitoridectomy (type 1) to infibulation or near-complete closure of the vulva (type 3), plus other practices such as pricking or cauterization (type 4). Over 230 million girls and women have undergone FGM in the 30-31 countries with systematic data, representing about 30 million more cases than in 2016, an approximate 15% increase. Each year, more than 4 million girls are estimated to be at risk of undergoing this practice. The cost to health systems for treating its complications is estimated at about 1.4 billion dollars annually and is expected to rise if its elimination is not accelerated.
Most cases are concentrated in Africa, with around 144 million survivors, followed by Asia with about 80 million, and the Middle East with more than 6 million, though it also exists in small communities on other continents and in migrant diasporas. Countries with the highest prevalence rates among women aged 15 to 49 include Somalia, Guinea, and Djibouti, where nearly all women in that age group have been mutilated. In other countries such as Sudan, Mali, Egypt, Eritrea, or Sierra Leone, the practice is also widespread, though with regional and ethnic variations. At the opposite end, countries like Uganda, Cameroon, or Niger show very low national prevalence rates, often concentrated in specific groups, reminding us that FGM is not a uniform feature of “Africa” but of certain communities. A recent report identified FGM presence in 94 countries, revealing its existence also in parts of Asia, the Middle East, Latin America, and migrant-receiving countries, though generally in small and little-visible communities.
In many communities, FGM operates as a social norm: families fear rejection, stigma, or that their daughters will not be able to marry if they do not undergo the rite. It is usually considered part of the transition to femininity and is associated with ideals of purity, family honor, and control of female sexuality, such as ensuring premarital virginity and marital fidelity. Although no major religious text mandates FGM, some people justify it in the name of religion, and the position of religious leaders can favor both its abandonment and its persistence. The weight of tradition, gender inequality, and the idea that “it has always been done this way” sustain the practice even among those who know its risks. In some contexts, so-called “medicalization” has increased: health personnel perform the mutilation thinking it makes it “safer” or for economic incentives, something the WHO condemns because it remains a violation of rights.
FGM has no health benefits and damages healthy genital tissue, interfering with basic bodily functions. Immediate complications include extreme pain, hemorrhages, infection, difficulty urinating, shock, and even death. In the long term, it can cause recurrent urinary and vaginal infections, painful periods, scars and keloids, pain during sexual intercourse, and reduced sexual response. Mutilated women have a higher risk of complicated childbirth, obstetric hemorrhages, cesareans, neonatal resuscitation, and newborn death. Psychologically, depression, anxiety, post-traumatic stress disorder, and a deep impact on self-esteem and body experience are frequent.
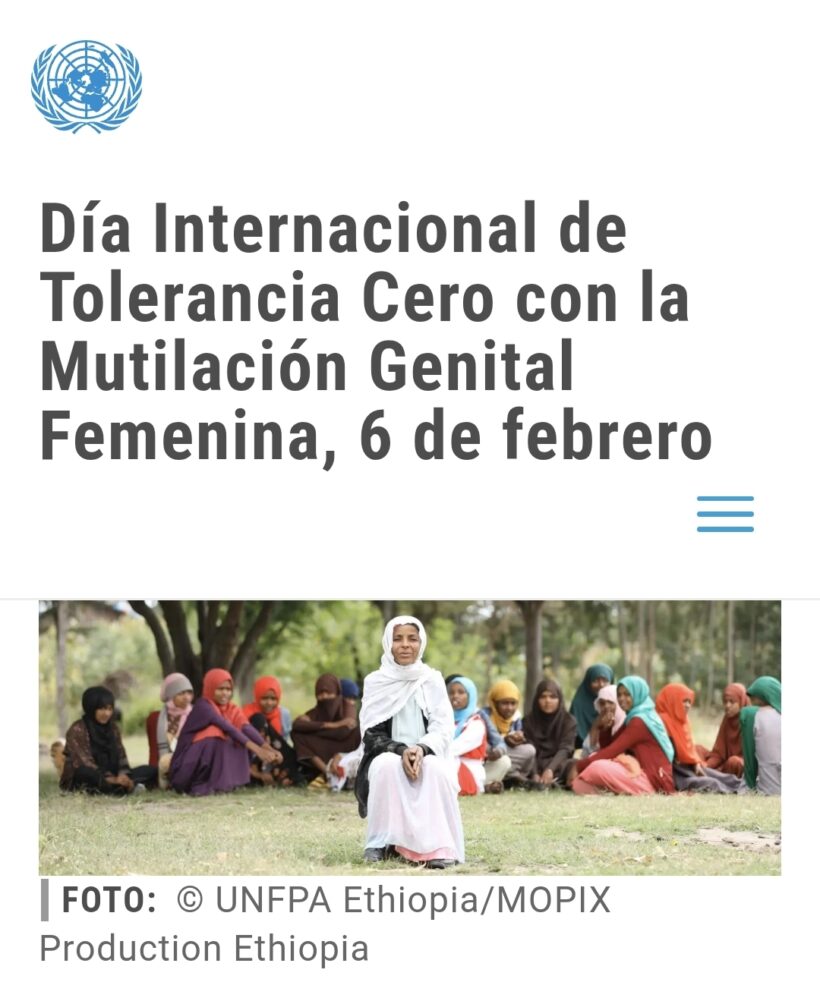
In 2008, the World Health Assembly approved a resolution calling for the elimination of FGM and coordinating actions in health, education, justice, finance, and women’s affairs. The WHO develops guidelines for health personnel, promotes that they refuse to perform FGM, and trains them to treat its complications and support survivors. UNICEF and the UN Population Fund (UNFPA) have led the Joint Programme to Eliminate FGM since 2008 in nearly 18 countries in Africa and the Middle East, working with governments, community leaders, and women’s organizations. This program promotes legal changes, awareness campaigns, comprehensive sexual education, psychosocial and medical support for survivors, and economic alternatives for those who previously depended on the practice for subsistence. According to recent data, UNFPA’s interventions in sexual and reproductive health contributed to 290,000 girls avoiding FGM in 2024, though the UN warns that the rate of abandonment would need to be dozens of times faster to meet the goal of eradicating it by 2030.
Numerous local and international NGOs, including survivor networks, African feminist organizations, and platforms like EndFGM, work from the ground documenting cases, pressing for effective laws, and developing community programs that challenge gender norms and offer alternative rites of passage. These organizations insist that the key is to empower girls and women themselves, involve men and religious leaders, and ensure laws are enforced alongside education, health services, and social protection.